Cirrhosis
Highlights
Causes of Cirrhosis
Cirrhosis is a liver disease characterized by permanent scarring of the liver that interferes with its normal functions. Causes include:
- Alcoholism
- Chronic hepatitis B and C
- Autoimmune hepatitis
- Bile duct disorders such as primary biliary cirrhosis and primary sclerosing cholangitis
- Nonalcoholic fatty liver disease (NAFLD), which includes nonalcoholic steatohepatitis (NASH)
- Metabolic disorders such as hemachromatosis, Wilson’s disease, and alpha-1 antitrypsin deficiency
- Prolonged exposure to certain chemicals and medications
Complications
Cirrhosis can cause many serious complications including:
- Ascites (fluid buildup in the abdomen)
- Variceal hemorrhage, severe bleeding from varices (enlarged veins in the esophagus and upper stomach)
- Spontaneous bacterial peritonitis, a severe infection of the membrane lining of the abdomen
- Hepatic encephalopathy, impaired mental function caused by buildup in the body of toxins such as ammonia
- Hepatocellular carcinoma, a type of liver cancer
- Hepatorenal syndrome, when kidney failure occurs along with severe cirrhosis
Dietary and Lifestyle Changes
All patients with cirrhosis can benefit from certain lifestyle interventions. These include:
- Stop drinking alcohol.
- Restrict dietary salt.
- Follow a good diet plan, which may include protein restriction.
- Get vaccinations for influenza, hepatitis A and B, and pneumococcal pneumonia (if recommended by your doctor).
- Inform your doctor of all prescription and nonprescription medications, and any herbs and supplements, you take or are considering taking.
Treatment
Cirrhosis is an irreversible condition. Treatment focuses on slowing the progression of liver damage and reducing the risk of further complications. Your doctor will treat any underlying medical conditions that are the cause of your cirrhosis. If liver damage progresses to liver failure, patients may be candidates for liver transplantation. Liver donations can come from either a cadaver or from a living donor. Patients with cirrhosis who have a liver transplant have very good chances for survival.
Introduction
Cirrhosis is an irreversible result of various disorders that damage liver cells over time. Eventually, damage becomes so extensive that the normal structure of the liver is distorted and its function is impaired.
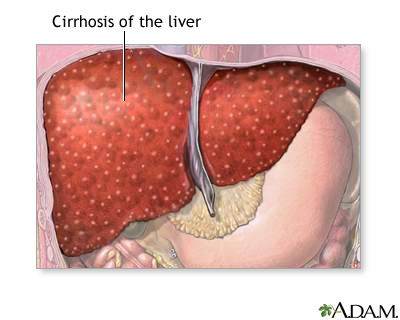
Scarring. The main damage in cirrhosis is triggered by scarring (fibrosis) that occurs from injuries due to alcohol, viruses, or other assaults. The scar tissue and other changes in liver cells gradually replace healthy liver tissue and act like small dams to alter the flow of blood and bile in and out of the liver.
Altered Blood and Bile Flow. The changes in blood and bile flow have significant consequences, with both the liver and other organs responding to the altered flow:
- The small blood vessels and bile ducts in the liver itself narrow (constrict). Blood vessels in other organs, including the kidney, also narrow.
- Blood flow coming from the intestine into the liver is slowed by the narrow blood vessels. It backs up through the portal vein and seeks other routes.
- Enlarged, abnormally twisted and swollen veins called varices form in the stomach and lower part of the esophagus to transport the blood diverted from the liver.
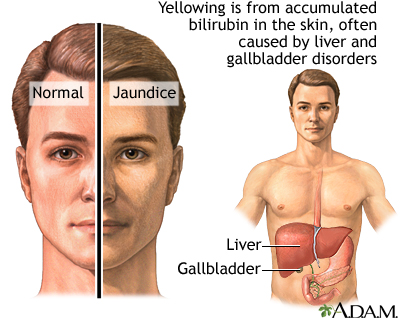
- Bilirubin also builds up in the bloodstream, resulting in jaundice, a yellowish cast in the skin and eyes, as well as dark-colored urine.
- Fluid buildup in the abdomen (called ascites), and swelling in the legs (edema) are common.
Functions of the Liver
The liver is the largest internal organ in the body. In the healthy adult, it weighs about 3 pounds. The liver is wedge-shaped, with the top part wider than the bottom. It is located right below the diaphragm and occupies the entire upper right quadrant of the abdomen.
The liver performs over 500 vital functions. Damage to the liver can impair these and many other processes. Among them are the following:
Processing Healthful Nutrients. The liver processes all of the nutrients the body requires, including proteins, glucose, vitamins, and fats.
Producing Proteins The liver is the body’s “factory” where many important proteins are made. The blood protein albumin is one example that is often underproduced in patients with cirrhosis.
Producing Bile. The liver produces bile, a green-colored fluid that helps the body absorb fats and fat-soluble vitamins. Bile contains bilirubin, a yellow-green pigment produced from the breakdown of hemoglobin, the oxygen-carrying component in red blood cells. Bile also contains bile salts, fatty acids, cholesterol, and other substances.
Bile travels from the liver to the gallbladder, where it is stored until after a meal. It is then secreted into the intestines where it helps digest fat. Because bile can also travel directly from the liver to the intestines, patients who have had their gallbladders removed can still absorb fat normally.
Eliminating Toxins. One of the liver's major functions is to render harmless potentially toxic substances, including alcohol, ammonia, drugs, and harmful by-products of digestion.
Structure of the Liver
The vital processes the liver performs rely on well-organized liver architecture.
The basic building blocks of the liver are the following structures:
- Bile ducts
- Blood vessels
- Working liver tissue (called the parenchyma)
- Supportive (connective) tissue
The liver is a built on a framework of lobes:
- Lobes. The liver is divided into two major lobes, a right and a smaller left, which are separated by tough, fibrous connective tissue.
- Lobules. The liver's two major lobes contain about 100,000 smaller lobes, called lobules. Each lobule contains microscopic columns of liver cells and blood vessels. Bracing the corners of each lobule column are an artery and a vein that carry blood and a bile duct that drains bile.
- Bile ducts. The bile ducts in the column corners collect bile draining from tiny canals around the liver cells. These ducts eventually join to form the large common bile duct that leads from the liver to the gallbladder.
- Arteries and veins. The arteries bring oxygen-rich blood to nourish the liver cells. The veins supply the liver cells with blood containing the nutrients and toxins that the liver cells process. A central vein runs through each column and collects the processed blood from both sources. These veins join to form the hepatic vein.
The Liver's Blood Supply. The liver is rich in blood. Its vessels contain about a pint, or 13% of the body's supply. It gets its blood from two large vessels, the hepatic artery and the portal vein, and is drained of blood by the hepatic vein. (The word "hepatic" derives from the Latin word for liver.)
The hepatic artery. This artery carries blood from the heart directly to the liver. This blood nourishes the liver.
The portal vein. The portal vein carries blood that has circulated through the stomach, spleen, and intestine to the liver. The liver processes this blood, extracting nutrients and toxins.
The hepatic vein. This vein carries blood away from the liver and connects to the inferior vena cava, a large vein that carries blood back to the heart.
Causes
Several processes can lead to cirrhosis.
Alcoholism
Chronic alcoholism particularly endangers the liver by causing alcoholic liver disease (also called alcohol-induced liver disease). Alcoholic liver disease includes fatty liver (build-up of fat cells in the liver), alcoholic hepatitis (inflammation of the liver caused by heavy drinking), and alcoholic cirrhosis. Alcoholic cirrhosis is the primary type of cirrhosis in the U.S. It develops in 10 - 20% of heavy drinkers, usually after 10 - 15 years of heavy alcohol consumption. People who drink heavily and who also have hepatitis C are at particular risk of developing cirrhosis. In the liver, alcohol converts to toxic chemicals that trigger inflammation and tissue injury, which lead to cirrhosis.
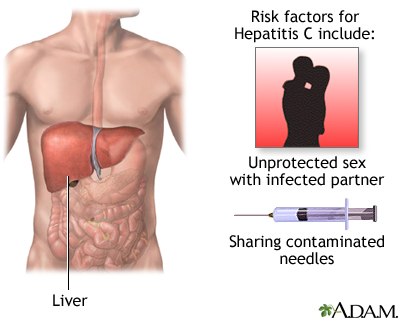
Chronic Viral Hepatitis
Chronic viral hepatitis, both hepatitis B and hepatitis C, is another primary cause of cirrhosis. Chronic hepatitis C is a more common cause of cirrhosis in developed countries, while hepatitis B is a more common cause of cirrhosis worldwide, especially in sub-Saharan Africa and parts of Asia. People with chronic hepatitis B who are co-infected with hepatitis D are especially at risk for cirrhosis. The longer a patient has had chronic hepatitis, the greater the risk for eventually developing cirrhosis.
Hepatitis viruses can produce inflammation in liver cells, causing injury or destruction. If the condition is severe enough, the cell damage becomes progressive, leading to scar tissue in the liver. In advanced cases, the liver shrivels in size, a condition called postnecrotic or posthepatic cirrhosis.
Autoimmune Hepatitis
Autoimmune hepatitis, like other autoimmune disorders, develops when a misdirected immune system attacks the body's own cells and organs. People who have autoimmune hepatitis also often have other autoimmune conditions, including systemic lupus erythematosus, rheumatoid arthritis, Sjögren syndrome, scleroderma, inflammatory bowel disease, glomerulonephritis, and hemolytic anemia. Autoimmune hepatitis typically occurs in women ages 15 - 40.
Bile Ducts Disorders
Disorders that block or damage the bile ducts can cause bile to back up in the liver, leading to inflammation and cirrhosis. These diseases include primary biliary cirrhosis and primary sclerosing chlorangitis.
Primary Biliary Cirrhosis. Up to 95% of primary biliary cirrhosis (PBC) cases occur in women, usually around age 50. In people with PBC, the immune system attacks and destroys cells in the liver’s bile ducts. Like many autoimmune disorders, the causes of PBC are unknown.
Primary Sclerosing Cholangitis. Primary sclerosing cholangitis (PSC) is a chronic disease that mostly affects men, usually around age 40. The cause is unknown, but immune system defects, genetics, and infections may play a role.
Nonalcoholic Fatty Liver Disease (NAFLD) and Nonalcoholic Steatohepatitis (NASH)
Nonalcoholic fatty liver disease (NAFLD) resembles alcoholic liver disease, but it occurs in people who do not drink a lot of alcohol. NAFLD is the most common liver disease in the United States.
NAFLD is actually a progressive spectrum of liver diseases that include:
- Nonalcoholic fatty liver (NAFL), or fatty liver, is the earliest stage of NAFLD. It is marked by the presence of fat in the liver (steatosis), but liver damage has not occurred. While a fatty liver is not normal, NAFL is not considered a serious condition.
- Nonalcoholic steatohepatitis (NASH) is the next stage of NAFLD. NASH is characterized by liver inflammation and injury, as well as a fatty liver. NASH is dangerous because it can lead to the scarring of the liver associated with cirrhosis. NASH is one of the leading causes of cirrhosis.
- Cirrhosis is the final irreversible stage of NAFLD.
Obesity and type 2 diabetes are the two main causes of NAFLD. Metabolic syndrome is another major factor. Metabolic syndrome is a collection of risk factors that include abdominal obesity, unhealthy blood lipid levels, high blood pressure, and insulin resistance.
Nonalcoholic fatty liver disease is usually benign and very slowly progressive. But, in certain patients, it can lead to cirrhosis and eventual liver failure. NAFLD also increases the risk for heart disease, which is the leading cause of death for these patients.
Hereditary Disorders
Hemochromatosis. Hemochromatosis is a disorder of iron metabolism. This disease interferes with the way the body normally handles iron. People with hemochromatosis absorb too much iron from the food they eat. The iron overload accumulates in organs in the body. When excess iron deposits accumulate in the liver, they can cause cirrhosis.
Other Hereditary Disorders. Other inherited diseases that can cause cirrhosis include Wilson’s disease (which causes an accumulation of copper in the body), alpha-1 antitrypsin deficiency (a genetic disorder caused by defective production of a particular enzyme), and glycogen storage diseases (a group of disorders that cause abnormal amounts of glycogen to be stored in the liver).
Other Causes
- Schistosomiasis, a disease caused by a parasite found in the Asia, Africa, and South America.
- Long-term or high-level exposure to certain chemicals and drugs, including arsenic, methotrexate, toxic doses of vitamin A, and certain prescription medications.
Symptoms
Cirrhosis is divided into two stages: Compensated and decompensated.
- Compensated cirrhosis means that the body still functions fairly well despite scarring of the liver. Many people with compensated cirrhosis experience few or no symptoms.
- Decompensated cirrhosis means that the severe scarring of the liver has damaged and disrupted essential body functions. Patients with decompensated cirrhosis develop many serious and life-threatening symptoms and complications.
Early symptoms of compensated cirrhosis may include:
- Fatigue and loss of energy
- Loss of appetite and weight loss
- Nausea or abdominal pain
- Spider angiomas may develop on the skin. These are pinhead-sized red spots from which tiny blood vessels radiate.
As cirrhosis progresses to a decompensated stage, patients may develop the following symptoms:
- Fluid buildup in the legs and feet (edema) and in the abdomen (ascites). (Ascites is associated with portal hypertension, which is described in the Complications section of this report.)
- Jaundice. This yellowish cast to the skin and eyes occurs because the liver cannot process bilirubin for elimination from the body.
- Itching. Itching (pruritus) develops from buildup of bile products.
- The palms of the hands may be reddish and blotchy, a condition known as palmar erythema
- In men, swelling of breasts or shrinkage of the testicles may occur.
- Easy bruising and excessive bleeding may occur.
Complications
A damaged liver affects almost every bodily process, including the functions of the digestive, hormonal, and circulatory systems. Decompensated cirrhosis increases the risk of serious and potentially life-threatening complications. (Once decompensation occurs, mortality rates without liver transplantation can be as high as 85% within 5 years.) The most serious complications are those associated with portal hypertension (increased pressure in the portal vein that carries blood from the intestine to the liver). They include:
- Ascites (fluid buildup in the abdomen)
- Variceal hemorrhage (bleeding in the upper stomach and esophagus from ruptured blood vessels)
- Spontaneous bacterial peritonitis is a form of peritonitis (inflammation of the membrane that lines the abdomen), which is associated with ascites. Other bacterial infections are also a common complication of cirrhosis.
- Hepatic encephalopathy (brain dysfunction). Impaired brain function occurs when the liver cannot detoxify harmful substances, and can lead to coma.
Liver cancer is a serious long-term risk with cirrhosis. Other complications also occur.
Ascites
Ascites is fluid buildup in the abdominal cavity. It is uncomfortable and can impair breathing and other functions. Ascites is caused by a combination of portal hypertension (high pressure in the blood vessels of the liver) and low albumin levels. Albumin is a protein produced by the liver. Although ascites itself is not fatal, it is a marker for severe progression.
Hepatorenal syndrome occurs if the kidneys drastically reduce their own blood flow in response to the altered blood flow in the liver. It is a life-threatening complication of late-stage liver disease that occurs in patients with ascites. Symptoms include dark colored urine and a reduction in volume, yellowish skin, abdominal swelling, mental changes (such as delirium and confusion), jerking or coarse muscle movement, nausea, and vomiting.
Variceal Bleeding
One of the most serious consequences of portal hypertension is the development of varices, veins that enlarge to provide an alternative pathway for blood diverted from the liver. In most patients, they form in the esophagus. They can also form in the upper stomach. Varices pose a high risk for rupture and bleeding because they are thin-walled, twisted, and subject to high pressure. Variceal intestinal bleeding is a life-threatening event. Symptoms include vomiting blood or black and tarry stools.
Spontaneous Bacterial Peritonitis
Spontaneous bacterial peritonitis is a life-threatening bacterial infection of the membrane that lines the abdomen. The main symptoms include confusion and altered mental status, fever, chills, and abdominal pain.
Hepatic Encephalopathy
Mental impairment is a common event in advanced cirrhosis. In severe cases, the disease causes encephalopathy (impaired brain function), with mental symptoms that range from confusion to coma and death. Hepatic encephalopathy is caused by a buildup in the blood of harmful intestinal toxins, particularly ammonia, which then accumulate in the brain. Encephalopathy can be triggered by many different conditions including internal bleeding, infection, constipation, and dehydration.
Early symptoms of hepatic encephalopathy include confusion, forgetfulness, and trouble concentrating. Sudden changes in the patient's mental state, including agitation or confusion, may indicate an emergency condition. Other symptoms include fruity-smelling bad breath and tremor. Late-stage symptoms of encephalopathy are stupor and eventually coma.
Liver Cancer
People with cirrhosis have an increased risk for hepatocellular carcinoma, a type of liver cancer. Hepatitis B and C, alcoholism, hemochromatosis, and primary biliary cirrhosis -- all causes of cirrhosis -- are some of the major risk factors for liver cancer. Cirrhosis due to hepatitis C is the leading cause of hepatocellular carcinoma in the United States.
Other Complications
Kidney Failure. Portal hypertension and spontaneous bacterial peritonitis can cause several secondary complications, including kidney failure. Nonsteroidal anti-inflammatory drugs (NSAIDs) -- such as ibuprofen (Advil, Motrin, generic), naproxen (Aleve, generic), and aspirin -- can also cause kidney failure in patients with cirrhosis.
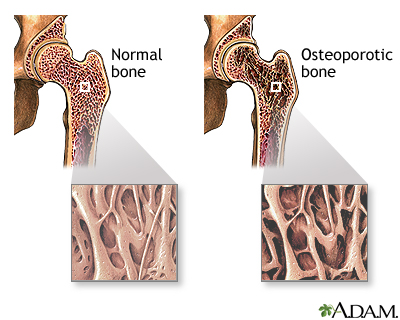
Osteoporosis. Many patients with cirrhosis develop osteoporosis, a bone-thinning disease. [For more information, see In-Depth Report #18: Osteoporosis.]
Insulin Resistance and Type 2 Diabetes. Cirrhosis often causes insulin resistance, a primary feature in type 2 diabetes. As insulin resistance progresses, it causes excess sugar (glucose) to build up in the blood, which leads to type 2 diabetes. In turn, type 2 diabetes is also a risk factor for nonalcoholic fatty liver disease, one of the causes of cirrhosis. [For more information, see In-Depth Report #60: Diabetes type 2.]
Heart Problems. Cirrhosis may increase the risk for heart failure and other cardiovascular complications.
Diagnosis
A physical examination may reveal the following in a patient with cirrhosis:
- The cirrhotic liver is firm and often enlarged in early stages of the disease. The liver may feel rock-hard. (In advanced stages of cirrhosis, the liver may become small and shriveled.)
- If the abdomen is swollen, the doctor will check for ascites by tapping the flanks and listening for a dull thud and feeling the abdomen for a shifting wave of fluid.
- The doctor will also check for signs of jaundice, muscle wasting, and (in male patients) breast enlargement.
A patient’s medical history is another indicator of the risk for cirrhosis. Patients with a history of alcoholism, hepatitis B or C, or certain other medical conditions are at high risk.
Other tests (blood tests, imaging tests, liver biopsy) may also be performed. The results of these tests along with the presence of specific complications (ascites and encephalopathy) are used for calculating the Child-Pugh Classification. This is a staging system (A to C) that helps doctors determine the severity of cirrhosis and predict the development of future complications.
Blood Tests
A patient’s medical history can reveal risk factors (such as alcoholism) that warrant screening for conditions such as hepatitis. Blood tests are also performed to measure liver enzymes associated with liver function. Enzymes known as aminotransferases, including aspartate (AST) and alanine (ALT), are released when the liver is damaged. Blood tests may also measure:
- Serum albumin concentration. Serum albumin measures the protein in the blood (low levels indicate poor liver function).
- Prothrombin time (PT). The PT test measures in seconds the time it takes for blood clots to form (the longer it takes the greater the risk for bleeding).
- Alkaline phosphatase (ALP). High ALP levels can indicate bile duct blockage.
- Bilirubin. One of the most important factors indicative of liver damage is bilirubin, a red-yellow pigment that is normally metabolized in the liver and then excreted in the bile. In patients with hepatitis, the liver cannot process bilirubin, and blood levels of this substance rise, sometimes causing jaundice.
Imaging Tests
Magnetic resonance imaging (MRI), computed tomography (CT), and ultrasound are all imaging techniques that are useful in detecting and defining the complications of cirrhosis, such as ascites and hepatocellular carcinoma. These imaging tests can also provide information on the extent of liver damage.
Liver Biopsy
A liver biopsy is the only definite method for confirming a diagnosis of cirrhosis. It also helps determine its cause, treatment possibilities, the extent of damage, and the long-term outlook. For example, patients with chronic hepatitis C who show no significant liver scarring when biopsied may have a low risk for cirrhosis.
A biopsy involves a doctor inserting a thin biopsy needle, guided by ultrasound, to remove a small sample of liver tissue. Local anesthetic is used to numb the area. Patients may feel pressure and some dull pain. The procedure takes about 20 minutes to perform.
The biopsy may be performed using various approaches, including:
- Percutaneous Liver Biopsy. This approach uses a needle inserted through the skin over the liver area to obtain a tissue sample from the liver. Various forms of needles are used, including those that use suction or those that cut out the tissue. This approach should not be used in patients with bleeding problems, and it must be used with caution in patients with ascites or severe obesity.
- Transjugular Liver Biopsy. This approach uses a catheter (a thin tube) that is inserted in the jugular vein in the neck and threaded through the hepatic vein (which leads to the liver). A needle is passed through the tube, and a suction device collects liver samples. This procedure is risky but may be used for patients with severe ascites.
- Laparoscopy. This procedure requires a small abdominal incision through which the doctor inserts a thin tube that contains small surgical instruments and a tiny camera to view the surface of the liver. This is generally reserved for staging liver cancer or for ascites of unknown cause.
Other Tests Used to Detect Complications of Cirrhosis
Endoscopy. Some doctors recommend endoscopy for patients newly diagnosed with mild-to-moderate cirrhosis in order to screen for esophageal varices. (These are enlarged veins in the esophagus that increase the risk for bleeding). In this test, a fiber-optic tube is inserted down the throat. The tube contains tiny cameras to view the inside of the esophagus, where varices are most likely to develop.
Paracentesis. If ascites is present, paracentesis is performed to determine its cause. This procedure involves using a thin needle to withdraw fluid from the abdomen. The fluid is tested for different factors to determine the cause of ascites:
- Bacteria cultures and white blood cell counts. (These are used to diagnose infection.)
- Protein levels. Low levels of protein in the fluid plus a low white blood cell count suggest that cirrhosis is the cause of the ascites.
Tests for Liver Cancer. Some doctors will screen patients with cirrhosis every 6 months to check for the development of liver cancer (hepatocellular carcinoma). To do this, a doctor will use both a blood test to check for levels of alpha-fetoprotein and an imaging test (ultrasound, MRI, or CT scan).
Treatment
Cirrhosis is an irreversible condition. Treatment goals are to slow the progression of liver damage and reduce the risk of further complications. There are currently no drugs available to treat liver scarring, although researchers are investigating various anti-fibrotic drugs.
Dietary and Lifestyle Changes
All patients with cirrhosis can benefit from certain types of lifestyle interventions. These include:
- Stop drinking alcohol. It is very important for people with cirrhosis to completely abstain from alcohol.
- Restrict dietary salt. Sodium (salt) can increase fluid buildup in the body. Eating a variety of foods every day can help you limit the amount of salt you are getting. It is best to eat fresh vegetables and fruits whenever possible and to avoid eating processed foods.
- Eat a healthy diet. People with cirrhosis are typically malnourished and require increased calories and nutrients. (Excess protein, however, can trigger hepatic encephalopathy.) They also need to avoid certain foods, such as raw seafood or shellfish, which carry risks of blood poisoning (septicemia). A dietician can provide dietary guidelines.
- Get vaccinated. Patients with cirrhosis should ask their doctors which vaccinations (such as hepatitis A, hepatitis B, influenza, pneumococcal pneumonia) they need.
- Discuss all medications with your doctor. Before you take any medications, (including nonprescription pain relievers such as acetaminophen), ask your doctor if they are safe for you. Liver damage affects the metabolism of drugs. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, and naproxen should not be used by patients with cirrhosis as they can trigger bleeding, worsen the condition, and potentially cause kidney failure.
- Inform your doctor of any herbs or supplements you are considering taking. Certain types of herbal remedies (kava, chaparral, kombucha mushroom, mistletoe, pennyroyal, and some traditional Chinese herbs) can increase the risk for liver damage. Although some herbs, such as milk thistle (silymarin) have been studied for possible beneficial effects on liver disease, there is no scientific evidence to show that they can help.
Recognizing Signs of Dangerous Complications
Patients with cirrhosis are susceptible to infections and bleeding, both of which can be life threatening. Contact your doctor’s office or go to the emergency room if you experience any of the following symptoms:
- Fever (temperature greater than 101 °F)
- Confusion that is new or suddenly becomes worse
- Vomiting more than once a day
- Rectal bleeding, black, tarry stools, vomiting blood or dark “coffee ground” material, or blood in the urine
- Diarrhea
- Abdominal or chest pain
- Shortness of breath
- Abdominal swelling or ascites that is new or suddenly becomes worse
- Jaundice (yellowing skin or eyes) that is new or suddenly becomes worse
Treatment of Underlying Conditions
Treatment for cirrhosis depends on the cause of cirrhosis.
Chronic Hepatitis. Many types of antiviral drugs are used to treat chronic hepatitis B, including pegylated interferon, nucleoside analogs, and nucleotide analogs. Patients with chronic hepatitis C are treated with combination therapy with pegylated interferon and ribavarin. In 2011, two new drugs – telaprevir (Incivek) and boceprevir (Victrelis) – were approved for use with hepatitis C combination therapy. [For more information, see In-Depth Report #59: Hepatitis.]
Autoimmune Hepatitis. Autoimmune hepatitis is treated with the corticosteroid prednisone and also sometimes immunosuppressants, such as azathioprine (Imuran).
Bile Duct Disorders. Ursodeoxycholic acid (Actigall, generic), also known as ursodiol or UDCA, is used for treating primary biliary cirrhosis but does not slow the progression. Itching is usually controlled with cholesterol drugs such as cholestyramine (Questran, generic) and colestipol (Colestid). Antibiotics for infections in the bile ducts and drugs that quiet the immune system (prednisone, azathioprine, cyclosporine, methotrexate) may also be used. Several surgical procedures may also be tried to open up the bile ducts.
Nonalcoholic Fatty Liver Disease (NAFLD) and Nonalcoholic Steatohepatitis (NASH). Weight reduction through diet and exercise, and diabetes and cholesterol management are the primary approaches to treating these diseases.
Hemochromatosis. Hemachromatosis is treated with phlebotomy, a procedure that involves removing about a pint of blood once or twice a week until iron levels are normal.
Treatment of Complications
Treatment of Ascites
First-line treatment of patients with ascites (fluid accumulation in the abdomen) involves:
- Dietary salt restriction (generally less than 1,500 mg/day of sodium)
- Drug treatment with diuretics, usually spironolactone (Aldactone, generic) and furosemide (Lasix, generic).
- Complete abstention from alcohol
- Fluid restriction is usually not necessary unless sodium levels in the blood are low.
Treatment for Recurring or Refractory Ascites. Patients with ascites that does not respond to standard diuretics after a month (refractory ascites) may require procedures to reduce fluid:
- Large-volume paracentesis, (which involves using a thin needle to withdraw fluid from the abdomen), may be used for ascites refractory to medical treatment or when complications are present.
- Transjugular intrahepatic portosystemic shunt (TIPS) uses a stent placed in veins in the middle of the liver to keep open a passage connecting the hepatic and portal veins. This helps reroute blood around the scarred liver. In the procedure, a long needle is inserted into the jugular vein in the neck and passed down to the hepatic and portal veins. TIPS is used for patients with ascites unresponsive to treatment and those who may require a liver transplant. In general, TIPS should be a second-line option for ascites that does not respond to diuretics.
Treatment of Spontaneous Bacterial Peritonitis
Patients with ascites who have high white blood cell counts should receive intravenous antibiotic therapy (usually cefotaxime) or oral antibiotic therapy with ofloxacin. Patients who have had an episode of spontaneous bacterial peritonitis are treated with long-term antibiotic therapy of norfloxacin (Noroxin) or trimethoprim/sulfamethoxazole (Bactrim, Septra, generic) to prevent further infection.
Treatment of Hepatorenal Syndrome
Hepatorenal syndrome can occur in patients with ascites. This is a life-threatening condition in which kidney failure develops because of altered blood flow in the liver. Patients with hepatorenal syndrome are treated with intravenous infusion of albumin. Drug therapy includes oral midodrine (ProAmatine, generic) and octreotide (Sandostatin, generic). Studies suggest that the vasoconstrictor drug terlipressin, given in combination with albumin, may be helpful for treating hepatorenal syndrome.
Treatment of Hepatic Encephalopathy
The first step in managing encephalopathy (damage to the brain) is to treat any precipitating cause, such as:
- High ammonia levels
- Bleeding
- Low oxygen
- Dehydration
- Infection
- Use of sedatives
A protein-restricted diet may be used to lower ammonia production. The laxative lactulose, given as a syrup or enema, is used to empty the bowels and to help improve mental status. The antibiotic neomycin may be added for patients who do not improve with lactulose alone. Rifaximin (Xifaxan) is another antibiotic used for treatment of hepatic encephalopathy.
Treatment of Variceal Bleeding
Primary Prevention. Primary prevention means treating the varices (swollen or distended veins) before they have bled. Varices that are present in the esophagus, stomach, or intestines are always at risk of bleeding. Nonselective beta-blockers drugs, which are commonly used to treat high blood pressure, may be given to prevent bleeding. Propanolol (Inderal, generic) or nadolol (Corgard, generic) are the standard beta-blockers used for variceal prevention.
Patients with medium-to-large varices that have not bled may also be treated with a surgical procedure called endoscopic variceal ligation (EVL). EVL is also called band ligation. It involves inserting an endoscope or tube down through the esophagus. The equipment contains microcameras and tiny instruments. Latex bands are wrapped around the bleeding varices to shut off the blood supply.
Other types of therapies, (such as nitrate drugs, shunts, or sclerotherapy), are generally not recommended for primary prevention of variceal bleeding.
Treatment. When varices located in the digestive tract begin to bleed (variceal hemorrhage), it is considered an emergency situation. The first step is to immediately achieve normal blood clotting (hemostasis) in order to stop the current bleeding episode. Patients almost always need blood transfusions.
The primary treatment for variceal hemorrhage is drug therapy with ocreotide (Sandostatin, generic). This drug is given for 3 - 5 days after the bleeding began to reduce the risk for rebleeding. Endoscopic variceal ligation (described above) is usually the preferred method. An alternative procedure is endoscopic sclerotherapy. In endoscopic sclerotherapy, the endoscopic tube is inserted through the mouth and a sclerosant (a solution that toughens the tissue around the variceal blood vessels) is injected to stop the bleeding.
If these treatments do not control the bleeding, or bleeding recurs, a transjugular intrahepatic portosystemic shunt (TIPS) procedure is performed. (For more information on TIPS, see "Treatment of Ascites" above.) TIPS is not useful as the first choice for stopping an initial bleeding episode or for preventing rebleeding since it poses a high risk for encephalopathy.
Another procedure, called balloon tamponade, may be used to temporarily control bleeding prior to the TIPS procedure. Balloon tamponade is performed only for bleeding that cannot be controlled by drugs or endoscopy. It involves inserting a tube through the nose and down through the esophagus until it reaches the upper part of the stomach. A balloon at the tube's end is inflated and positioned tightly against the esophageal wall. It is usually deflated in about 24 hours. Balloon tamponade poses a risk for serious complications, the most dangerous being rupture of the esophagus.
Secondary Prevention. Patients who survive an episode of variceal bleeding need to be treated with drugs to prevent bleeding recurrence. Patients are prescribed either a combination of a nitrate drug (such as isosorbide, which is used to treat angina) and a nonselective beta-blocker (propanolol or nadolol) or a beta-blocker alone. Patients are also given several sessions of endoscopic variceal ligation over the course of several months. The TIPS procedure may be recommended for patients who experience recurrent bleeding despite drug and endoscopic therapy.
Liver Transplantation
When cirrhosis progresses to end-stage liver disease, patients may be candidates for liver transplantation. Patients with liver cancer that has not spread beyond the liver are also candidates for transplant.
Current 5-year survival rates after liver transplantation are about 75%. Patients report improved quality of life and mental functioning after liver transplantation. Patients should seek medical centers that perform more than 50 transplants per year and produce better-than-average results.
A scoring system called Model for End-Stage Liver Disease (MELD) is used to determine which patients are most in need of a donor liver. A MELD score predicts 3-month survival based on laboratory tests of creatinine, bilirubin, and blood-clotting time. Priority is given to patients who are most likely to die without a liver transplant.
Unfortunately, there are many more patients waiting for liver transplants than there are available organs. Patients may also want to consider living-donor liver transplantation. In living-donor transplantation, surgeons replace the patient’s diseased liver with a part of the liver taken from a donor. The donor’s liver regenerates to full size within a few weeks of surgery, and the recipient’s liver also regrows. This procedure produces excellent results for patients, but there are some risks for the donor.
Transplantation surgery generally takes 4 - 12 hours to perform, and patients stay in the hospital for up to 3 weeks after the surgery. Most patients return to normal or near-normal activities 6 - 12 months following the transplant. For the rest of their lives, patients need to take immunosuppressive medication to prevent rejection.
Liver Transplantation in Patients with Viral Hepatitis. One of the primary problems with performing liver transplantation in patients with hepatitis is recurrence of the virus after transplantation. Recurrence typically occurs with hepatitis C. Viral recurrence can also occur with hepatitis B. HepaGam B is an immune globulin preparation approved to prevent recurrence of hepatitis B after transplantation. Patients need to receive periodic HepaGam B injections on a lifelong basis.
Liver Transplantation for Patients with Primary Biliary Cirrhosis. Patients who require transplantation for primary biliary cirrhosis are those who develop major complications of portal hypertension and liver failure or who have poor quality of life and short survival without the procedure. Survival rates after transplantation are excellent.
Liver Transplantation for Patients with Autoimmune Hepatitis. The outlook is also good for patients who have autoimmune hepatitis who require a transplant. Survival rates are about 90% after 1 year, and 70 - 80% after 5 years. Rejection usually occurs in those patients whose immune systems are very compromised.
Liver Transplantation for Patients with Alcoholism. Liver transplantation is generally not recommended for patients with active alcohol or drug abuse addictions.
Resources
- www2.niddk.nih.gov -- National Institute of Diabetes and Digestive and Kidney Diseases
- www.aasld.org -- American Association for the Study of Liver Diseases
- www.liverfoundation.org -- American Liver Foundation
- www.gastro.org -- American Gastrointestinal Association
- www.cdc.gov/ncidod/diseases/hepatitis -- Centers for Disease Control and Prevention, Hepatitis
- www.hepfi.org -- Hepatitis Foundation International
- www.unos.org -- United Network for Organ Sharing
- www.organdonor.gov -- US government organ donor site
References
Berg CL, Gillespie BW, Merion RM, Brown RS Jr, Abecassis MM, Trotter JF, et al Improvement in survival associated with adult-to-adult living donor liver transplantation. Gastroenterology. 2007 Dec;133(6):1806-13. Epub 2007 Sep 14.
Brown RS Jr. Live donors in liver transplantation. Gastroenterology. 2008 May;134(6):1802-13.
Cárdenas A, Ginès P. Management of patients with cirrhosis awaiting liver transplantation. Gut. 2011 Mar;60(3):412-21. Epub 2010 Dec 30.
Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 2012 Jun;55(6):2005-23.
Chapman R, Fevery J, Kalloo A, Nagorney DM, Boberg KM, Shneider B, et al. Diagnosis and management of primary sclerosing cholangitis. Hepatology. 2010 Feb;51(2):660-78.
Chandok N, Watt KD. Pain management in the cirrhotic patient: the clinical challenge. Mayo Clin Proc. 2010 May;85(5):451-8. Epub 2010 Mar 31.
Garcia-Tsao G, Bosch J. Management of varices and variceal hemorrhage in cirrhosis. N Engl J Med. 2010 Mar 4;362(9):823-32.
Garcia-Tsao G, Lim JK; Members of Veterans Affairs Hepatitis C Resource Center Program. Management and treatment of patients with cirrhosis and portal hypertension: recommendations from the Department of Veterans Affairs Hepatitis C Resource Center Program and the National Hepatitis C Program. Am J Gastroenterol. 2009 Jul;104(7):1802-29. Epub 2009 May 19
Garcia-Tsao G, Sanyal AJ, Grace ND, Carey WD; Practice Guidelines Committee of American Association for Study of Liver Diseases; Practice Parameters Committee of American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Am J Gastroenterol. 2007 Sep;102(9):2086-102.
Ginès P, Schrier RW. Renal failure in cirrhosis. N Engl J Med. 2009 Sep 24;361(13):1279-90.
Gonzalez R, Zamora J, Gomez-Camarero J, Molinero LM, Bañares R, Albillos A. Meta-analysis: Combination endoscopic and drug therapy to prevent variceal rebleeding in cirrhosis. Ann Intern Med. 2008 Jul 15;149(2):109-22.
Lindor K. Ursodeoxycholic acid for the treatment of primary biliary cirrhosis. N Engl J Med. 2007 Oct 11;357(15):1524-9.
Lindor KD, Gershwin ME, Poupon R, Kaplan M, Bergasa NV, Heathcote EJ; American Association for Study of Liver Diseases. Primary biliary cirrhosis. Hepatology. 2009 Jul;50(1):291-308.
Marchesini G, Moscatiello S, Di Domizio S, Forlani G. Obesity-associated liver disease. J Clin Endocrinol Metab. 2008 Nov;93(11 Suppl 1):S74-80.
O'Leary JG, Lepe R, Davis GL. Indications for liver transplantation. Gastroenterology. 2008 May;134(6):1764-76.
Parikh S, Hyman D. Hepatocellular cancer: a guide for the internist. Am J Med. 2007 Mar;120(3):194-202.
Parikh S, Shah R, Kapoor P. Portal vein thrombosis. Am J Med. 2010 Feb;123(2):111-9.
Runyon BA; AASLD Practice Guidelines Committee. Management of adult patients with ascites due to cirrhosis: an update. Hepatology. 2009 Jun;49(6):2087-107.
Salerno F, Cammà C, Enea M, Rössle M, Wong F. Transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis of individual patient data. Gastroenterology. 2007 Sep;133(3):825-34. Epub 2007 Jun 20.
Schuppan D, Afdhal NH. Liver cirrhosis. Lancet. 2008 Mar 8;371(9615):838-51.
Udell JA, Wang CS, Tinmouth J, FitzGerald JM, Ayas NT, Simel DL, et al. Does this patient with liver disease have cirrhosis? JAMA. 2012 Feb 22;307(8):832-42.
|
Review Date:
12/26/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M. Health Solutions, Ebix, Inc. |






